DBS Surgery
Do you know that over 7 million people in India are affected by Parkinson’s disease? Despite advancements in medical treatment, many continue to suffer from severe symptoms and side effects of medicine as the disease progresses. Could Deep Brain Stimulation surgery in Mumbai be the breakthrough for this disease? Can DBS improve the quality of life and make them independent again??
Yes, this revolutionary procedure has transformed lives worldwide. This advanced procedure offers a new lease on life by effectively managing symptoms and improving the quality of life for those suffering from various neurological disorders.
What is Deep Brain Stimulation Surgery?
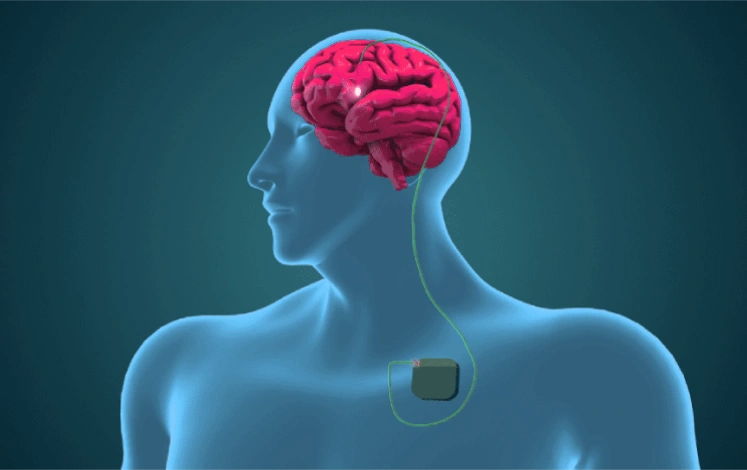
Deep Brain Stimulation (DBS) surgery involves implanting a thin electrode deep within the brain under local anaesthesia. The electrode is permanently left in place in the brain and connected to a small pacemaker (IPG) implanted in the chest. No leads or implants are seen outside the body. The IPG is programmed with the help of a remote, and it controls the abnormal functions of the brain like motor symptoms like tremors, rigidity and slowness.

Who Is a Good Candidate for Deep Brain Stimulation?
- Refractory Conditions: Individuals whose movement or psychiatric symptoms (e.g., Parkinson’s, essential tremor, dystonia, chorea, OCD, or severe depression) no longer respond adequately to medications or other therapies.
- Significant Daily Impact: Those whose quality of life is markedly reduced by symptoms affecting work, social interactions, and routine tasks.
- Clear Understanding: Patients who recognize that DBS manages symptoms rather than cures the underlying condition—and are aware of both the benefits and potential risks.
- Medical Readiness: Candidates without severe comorbidities (e.g., advanced dementia, active psychosis, untreated infections) that could complicate surgery or post-operative recovery.
- Commitment to Care: They can follow pre- and post-surgical advice, attend programming sessions to fine-tune the device, and maintain realistic expectations for outcomes.
Overall, a multidisciplinary evaluation helps confirm whether a patient’s specific symptoms and medical status align with.
How Does Deep Brain Stimulation Work?
DBS involves implanting thin electrodes in specific regions of the brain depending on the underlying disease. These electrodes are connected to a neurostimulator placed under the skin of the chest. The device sends controlled small electrical pulses to regulate neural activity, reducing symptoms like tremors, muscle rigidity, and uncontrollable movements.
What Is the Ideal Time to Undergo DBS Surgery?
This differs from disease to disease, for example, in Parkinson’s, the earlier the surgery the better and the greater the results, but for psychiatric disorders, this is considered the last option. We describe various neurological disorders where DBS is indicated.
In the early years, Parkinson’s disease can typically be managed with medications. However, as the disease progresses, side effects such as motor fluctuations, dyskinesias, and hallucinations become more prominent.
At this stage, increasing the medication dosage often leads to more side effects than benefits. This phase usually occurs around four to six years after the onset of the disease. Therefore, DBS surgery should be considered when medication doses are gradually increasing or symptoms are no longer adequately controlled by three doses of medications in a day and when the side effects of a medication begin to affect the patient’s quality of life.
For Dystonia, DBS can be considered as the first option as medicines and botox are not very effective and provide only a short-term partial relief. DBS can provide an excellent cure for dystonia and restore the functioning of the body part involved. Few of the common dystonias treated with DBS are cervical dystonia, generalized dystonia, orofacial dystonia, writer’s cramp, etc.
For Chorea also DBS can be considered as an option when the medicines stop working and provide an excellent control of the movements. In diseases like Huntington’s chorea, neuroacanthocytosis chorea, DBS provide excellent relief. In Hungtingtons, DBS provides control of only chorea movements and not the other symptoms of Huntingtons like memory loss.
DBS is considered as the last option in refractory cases for diseases like epilepsy, status epilepticus, OCD, Depression, Schizophrenia, Addiction, and Alzheimer’s. Refractory epilepsy is controlled by 70% and the drugs are also reduced by 70-80%. Similarly psychiatric disorders are also controlled by 60-80% and the drugs are reduced significantly by 70-80%.
What Makes DBS Superior to Other Treatments?
Compared to ablative surgeries, DBS is minimally invasive and reversible. As this is an awake surgery, the results of the surgery are appreciated and confirmed by the patient during the surgery. It offers significant symptom improvement with lower risks of permanent side effects. The advancement in technology has made this surgery completely safe and has minimized the side effects and complications to almost less than 2%. Patients can experience improved motor functions, reduced tremors, and a better quality of life.
What Conditions Can DBS Treat?
DBS is a versatile treatment option used to manage multiple conditions, including:
- Parkinson’s disease (to control tremors, rigidity, and dyskinesias)
- Essential tremor (to reduce shaking in the hands, head, or voice)
- Dystonia (to alleviate painful muscle contractions)
- OCD (to reduce intrusive thoughts and compulsions)
- Severe depression (to help regulate mood)
Is This Surgery Risky and Not Advised for Elderly Patients?
Many elderly patients are worried about undergoing this procedure as this is being done in the brain and most of them have many co-morbidities like coronary artery disease, diabetes, hypertension, knee arthritis and back pain.
The safety of DBS surgery depends on the surgeon’s expertise and experience and all the precautions taken before the surgery. DBS is a safe and straightforward procedure, and our team specializes in handling elderly patients with multiple comorbidities. As mentioned earlier this is a non-destructive surgery and involves only the placement of the thin electrodes in the brain. Hence with all the safety precautions, this procedure can be safely executed in all elderly patients.
If a patient cannot tolerate local anesthesia, we can perform the procedure under conscious sedation. We also ensure that both the patient and their family are well-prepared, making the surgical experience as comfortable and safe as possible. Our research comparing elderly and younger patients operated at our center found no increase in complication rates, and the improvement in Parkinson’s disease symptoms was similar across both groups.
On the second day of DBS surgery, a patient can do all his personal care activities and have a normal diet. It involves a very short recovery period.
What Is Programming, and How Important Is It for the Outcome of Surgery?

Programming is the key to success in DBS surgery. Proper knowledge and expertise in pacemaker programming are crucial to achieve the best results.
- If the device is not programmed correctly, the desired benefits of the surgery may not be achieved.
- Our team has over 2000 hours of programming experience, allowing us to immediately assess how each program setting affects the patient and offer the best possible adjustments.
What Are the Different Types of Implants? What Needs to Be Checked Before Selecting One?
There are two major companies that provide DBS implants in India:
✔ Medtronic
✔ Boston Scientific
When choosing the best DBS implant, four key factors need to be considered:
- MRI Compatibility – Ensuring the implant allows future MRI scans if needed.
- Rechargeable vs. Non-Rechargeable – Whether you prefer a rechargeable device or one that needs battery replacement over time.
- Battery Life – Longer battery life reduces the need for frequent replacements and is cost-effective.
- Advanced Programming Features – Some implants offer additional customization options for better symptom control in the advanced disease stages.
The best implant choice varies for each patient, depending on their disease condition and needs. Your surgeon is the best person to guide you in making the right selection.
Can You Describe the Entire DBS Procedure?
- Two-Step Surgery:
- Step 1: Implantation of an electrode deep within the brain under local anesthesia.
- Step 2: Implantation of an IPG (pacemaker) in the chest.
- Pre-Surgical Assessments (Day 1 & 2):
- Extensive Parkinson’s Disease evaluations, video recordings, and patient counseling.
- MRI scan under sedation or general anesthesia.
- Electrode Implantation (Day 3):
- Surgery performed under local anesthesia.
- Patient remains awake for real-time stimulation trials to confirm electrode placement.
- Pacemaker Implantation (Day 4):
- Done under general anesthesia.
- Post-Surgery programming of the device and exercise training (Day 5 to 10 days):
- Hospital stay continues until suture removal and device programming are completed.
- Patients are monitored for any immediate post-surgical adjustments and fine-tuning.
- Patients are given speech therapy, gait, balance, and posture training, daily, physiotherapy to build muscle tone and strength, and psychological counseling for mental illness.
Is the Surgery Painful? Will I Be Sedated?
Initially, you may feel a minor pinprick when local anesthesia is administered. However, once the local anesthesia takes effect, you will not feel any pain during the surgery.
You will be aware that the procedure is taking place, but we will keep you informed throughout to ensure your comfort and confidence. Our experience shows that none of our patients have found the surgery to be traumatic. You will not be sedated during the procedure.
What Precautions Will I Have to Take After DBS Surgery?
After surgery, we will provide you with a detailed list of dos and don’ts to safeguard the DBS pacemaker. However, in general, you can continue with all normal activities, such as:
- Swimming
- Dancing
- Jogging
- Exercise
- Using a cell phone
- Using a microwave oven
- Driving
What Would Be the Follow-Up Schedule After Surgery?
We have a track record of programming most patients before discharge, ensuring minimal follow-up requirements.
- More than 50% of patients do not require follow-ups for up to 6 months 2 years.
- If needed, most programming can be done on an outpatient basis, without requiring hospital admission.
How Long Does Recovery Take After DBS Surgery?
Recovery from DBS surgery generally takes a few days Patients may experience temporary side effects such as swelling, headaches, or mild discomfort at the incision site. These issues are usually resolved with medication and wound care.
What are the Success Rates of DBS?
The success of DBS largely depends on the patient’s condition, the accuracy of electrode placement, and post-operative care. Research indicates:
- 80-90% tremor reduction for essential tremor
- 80-90% motor function improvement for Parkinson’s disease
- 40-70% symptom improvement for OCD, dystonia, and epilepsy
What Are the Risks of DBS Surgery?
- DBS surgery is safe when performed by experienced specialists like functional neurosurgeon, with minimal risks. Our analysis shows that the risk of major complications is less than 2%, which compares favorably with the best centers worldwide.
- As a patient, it is essential to evaluate the risk-benefit ratio before undergoing the procedure. The risks associated with DBS surgery decrease with the surgeon’s experience and expertise. Just like an experienced and well-trained driver is less likely to make mistakes than a new driver, an experienced neurosurgeon ensures greater precision and safety during the procedure. At the same time the driver must not be too old that he is not aware of handling modern high-end cars like the DBS device where the technology is rapidly changing every 2 years and involves a lot of computer software handling.
What Does Life After DBS Look Like?
Patients who undergo DBS often experience significant improvements in their quality of life. In Parkinson’s disease, enhanced mobility, reduced symptoms, and improved emotional well-being are commonly observed. Many patients also report increased family interactions, greater participation in social gatherings, and a noticeable boost in overall happiness, as shared by their relatives. However, patients must continue with regular exercise, follow-ups, device programming, and lifestyle adjustments.
Is DBS a Cure for Neurological Disorders?
DBS is not a cure but a highly effective symptom management tool. It can drastically improve daily functioning and reduce reliance on medications. All the high medicine side effects can be avoided. However, patients need ongoing medical supervision to maintain optimal results.
How Effective Is DBS for Parkinson’s Disease?
DBS is highly effective in managing Parkinson’s disease symptoms. It significantly reduces motor fluctuations, improves movement control, and enhances the overall quality of life. Studies show that DBS can lead to a 80-90% improvement in motor function, reducing tremors, stiffness, and dyskinesias. Additionally, it allows for a 60-80% reduction in Parkinson’s medications, minimizing drug-related side effects. It all depends on how early the DBS surgery is done. The earlier the surgery, the better the outcomes, leading to greater benefits and a significant reduction in medication. It also helps slow the progression of Parkinson’s disease.
How Effective Is DBS for Parkinson’s Disease?
The cost of Deep Brain Stimulation surgery in Mumbai can range from ₹14 lakhs to ₹25 lakhs, depending on several factors:
- The specific neurological condition being treated
- Complexity and duration of the surgical procedure
- Type and model of the neurostimulator device used
- Pre- and post-operative care, including follow-up consultations and programming
Patients should also factor in additional expenses such as hospital stay, diagnostic tests, and medication.
What are the Benefits of DBS Surgery?
Increased “ON” Period: Improves the duration when patients are fully functional without medication side effects, extending the good period to 70-80% of the day.
Reduction in Medication Dependency: Helps in reducing the need for Parkinson’s medications by 60-70%, minimizing drug-related side effects.
Better Motor Control: Offers significant improvement in motor fluctuations, tremors, dyskinesias, and rigidity, leading to smoother movements.
Reduction in Hallucinations: Helps in managing hallucinations and other cognitive issues that may arise due to medication or disease progression.
Mood Enhancement: Reduces depression and anxiety, leading to an overall positive emotional state.
Weight Gain: Patients often experience healthy weight gain, which is beneficial for overall well-being.
Improved Quality of Life: Enhances daily functioning, social interactions, and independence.
Personalized Outcomes: Since results vary from patient to patient, it is crucial for the surgeon to assess individual conditions and set realistic expectations.
Expertise Matters: Not all centers have adequate experience, so choosing a skilled and experienced surgeon who has complete knowledge of presurgical evaluation, surgical technique, post-surgery care, medicine adjustments, device programming and rehabilitation exercises is essential for better outcomes.
Who is the Best Deep Brain Stimulation Specialist in Mumbai?
Choosing the right functional neurosurgeon for Deep Brain Stimulation (DBS) can significantly affect treatment outcomes and overall quality of life. Dr. Manish Baldia stands out in Mumbai for his specialized experience, cutting-edge techniques, utilization of advanced technology, and patient-focused approach. Dr. Baldia takes complete responsibility for the outcome, unlike other centers.
- Extensive Experience: With 11 years in neurosurgery, Dr. Baldia has honed his skills across various functional neurosurgical procedures.
- Top-Tier Credentials: His qualifications include an MCh from CMC Vellore, a Fellowship in Functional Neurosurgery, and EEPIN (London).
- Diverse Expertise: In addition to DBS, he handles complex cases such as Epilepsy surgery, lesionectomy, pallidotomy, diaphragm pacing, pain relieving surgeries and Vagal Nerve Stimulation.
- Conditions Treated: Dr. Baldia also specializes in Cranioplasty, Brain and spine tumors, spine surgeries, spondylosis, trigeminal neuralgia, peripheral neuropathy pain, urinary incontinence. Patient-Centric Care: Working at Apollo Hospitals CBD Belapur, he emphasizes personalized treatment plans and thorough follow-up.
If you seek an expert who combines technical mastery with compassionate care, Dr. Manish Baldia is often recognized as one of Mumbai’s leading neurosurgeons for DBS and other advanced neurosurgical interventions. Book your appointment today.

Case series: 1
A 65-year-old male with advanced Parkinson’s Disease presented with severe tremors, rigidity, and motor fluctuations unresponsive to medication. Preoperative imaging and evaluations confirmed eligibility for Deep Brain Stimulation (DBS). The procedure, was performed in one of the reputed hospitals by a senior neurosurgeon leading to significant side effects after surgery like loss of memory, difficulty in walking and behaviour changes.
Before and After DBS Surgery
- Before DBS Surgery: Severe tremors, rigidity, and limited mobility.
- After DBS Surgery: Minimal improvement in symptoms with more side effects and new symptoms like memory loss, and difficulty in walkingThe video “Advance Technology to Rescue a Failed DBS Surgery” highlights the correction of a failed DBS procedure using advanced imaging and real-time brain mapping by Dr Manish Baldia. It showcases how the knowledge of electro-neurophysiology and utilization of advanced software for brain nerve fibre tracking helped in avoiding a re-surgery for misplaced electrodes. Post-programming and treatment, the patient showed immediate improvements, reinforcing the effectiveness of neuromodulation in managing Parkinson’s Disease and movement disorders.
Case Series : 2
A 68-year-old male with advanced Parkinson’s Disease struggled with severe tremors, stiffness, and mobility issues that worsened despite medication. After evaluation, he underwent Deep Brain Stimulation (DBS) performed by Dr. Manish Baldia, involving precise electrode placement in the subthalamic nucleus (STN) to restore motor function. The video “DBS for Parkinson’s Disease” documents the patient’s preoperative difficulties, the meticulous surgical process, and the striking postoperative improvements. Following the procedure, his tremors significantly reduced, movement became smoother, and his independence was restored. The video effectively highlights how DBS, under expert guidance, transforms the lives of Parkinson’s patients by providing enhanced motor control and a better quality of life.